In this blog series focused on osteoimmunology, we explored the fascinating intersection of bone biology and the immune system. Next, let’s consider how our understanding of the interplay between immune cells and bone tissue is contributing to new strategies to accelerate healing, prevent complications, and enhance overall skeletal health.
The Role of Osteoimmunology in Bone Healing
Five Osteoimmune Strategies to Improve Bone Health and Fracture Repair
Target Inflammatory Pathways
Inflammation is essential in fracture healing, but chronic inflammation can hinder bone repair. By modulating inflammatory cytokines like TNF-α and IL-6, scientists aim to support a more balanced immune response that supports healing, rather than impeding it (3). One of the many challenges of developing this type of therapy is finding a system to deliver a precise dose to a specific target to ensure localized effects without systemic side effects.
Leverage Immune Cells for Regeneration
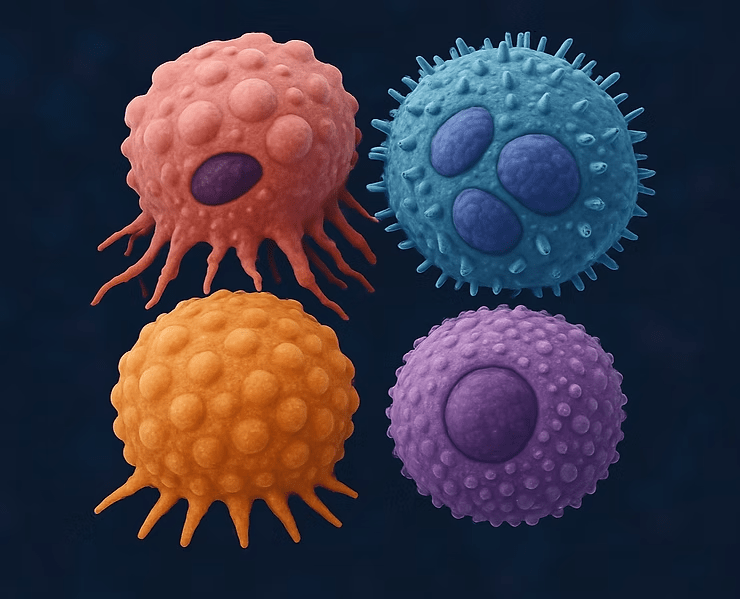
Macrophages, mast cells, and other immune cells play a pivotal role in fracture healing. Researchers hope that understanding the function of these cells will enable development of therapies to harness and enhance their regenerative capabilities.
As an example, CCR8+ regulatory T cells have been shown to migrate to the site of bone fracture, where they support bone repair through osteoprogenitor differentiation and secretion of progranulin. Progranulin is a secreted glycoprotein known to modulate inflammatory processes through TNF-α regulation, enhanced extracellular matrix synthesis, and is important in maintaining the osteoclast-osteoblast equilibrium (4-6). Potential targets for new therapies include methods to enhance T cell migration or increase progranulin secretion.
Optimizing the Bone Marrow Microenvironment
Bone marrow is a shared space for both skeletal and immune cells. A healthy bone marrow niche is better able to support bone remodeling and repair. By the same token, understanding the ramifications of bone marrow diseases or cancer treatments on bone biology is critical to maximizing bone health in these patients.
Osteoimmune-based Biologics
Innovative treatments, such as biologics that regulate the RANK/RANKL/OPG axis, are being explored to improve bone density and fracture healing. Many of these proteins and cytokines are found throughout the body, so designing precise and targeted delivery systems is key to the prevention of off-target effects. One example is denosumab, a monoclonal antibody that binds with high affinity to RANKL. This blocks the interaction of RANKL with RANK, thereby inhibiting osteoclast differentiation and activity. It is used in some cancer patients to prevent bone fractures (7,8).
Personalized Medicine Approaches
Since immune responses vary by age, sex, and genetic predisposition, personalized osteoimmune therapies could be the future of fracture repair (9).
Looking Ahead
References
Miron, R.J., Bohner, M., Zhang, Y., & Bosshardt, D. D. (2024). Osteoinduction and osteoimmunology: Emerging concepts. Periodontology 2000, 94(1), 9–26. https://doi.org/10.1111/prd.12519
Zhao, T., Chu, Z., Ma, J., & Ouyang, L. (2022). Immunomodulation Effect of Biomaterials on Bone Formation. Journal of Functional Biomaterials, 13(3), 103. https://doi.org/10.3390/jfb13030103
Xue, Pengfei, et al. “Material‐Mediated Immunotherapy to Regulate Bone Aging and Promote Bone Repair.” Small : Nano Micro, vol. 21, no. 11, 2025, https://doi.org/10.1002/smll.202409886
Chen R, Zhang X, Li B, Tonetti MS, Yang Y, Li Y, Liu B, Qian S, Gu Y, Wang Q, Mao K, Cheng H, Lai H, Shi J. Progranulin-dependent repair function of regulatory T cells drives bone-fracture healing. J Clin Invest. 2024 Nov 7;135(2):e180679. doi: 10.1172/JCI180679. PMID: 39509336; PMCID: PMC11735098.
Wang S, Zhang H, Zhu Y, Zhou X, Zhai H, He Q, Zhu X, Zhang Y. Progranulin Protects Against Osteoporosis by Regulating Osteoclast and Osteoblast Balance via TNFR Pathway. J Cell Mol Med. 2025 Feb;29(3):e70385. doi: 10.1111/jcmm.70385. PMID: 39910695; PMCID: PMC11798871.
6Wang X, Liang Y, Yang F, Shi Y, Shao R, Jing R, Yang T, Chu Q, An D, Zhou Q, Song J, Chen H, Liu C. Molecular mechanisms and targeted therapy of progranulin in metabolic diseases. Front Endocrinol (Lausanne). 2025 Apr 11;16:1553794. doi: 10.3389/fendo.2025.1553794. PMID: 40290306; PMCID: PMC12021630.
Mukherjee, R., Chang, C.-M., & Pati Pandey, R. (2023). Immunology and Osteoporosis: A New Frontier in Treatment. In R. K. Srivastava (Ed.), Osteoporosis—Pathophysiology, Diagnosis, Management and Therapy. IntechOpen. https://doi.org/10.5772/intechopen.1002916
Pietschmann, P., Mechtcheriakova, D., Meshcheryakova, A., Föger-Samwald, U., & Ellinger, I. (2016). Immunology of Osteoporosis: A Mini-Review. Gerontology, 62(2), 128–137. https://doi.org/10.1159/000431091
Molitoris, K.H., Huang, M. & Baht, G.S. Osteoimmunology of Fracture Healing. Curr Osteoporos Rep 22, 330–339 (2024). https://doi.org/10.1007/s11914-024-00869-z
© 2025 Molecular Matrix, Inc. All rights reserved.