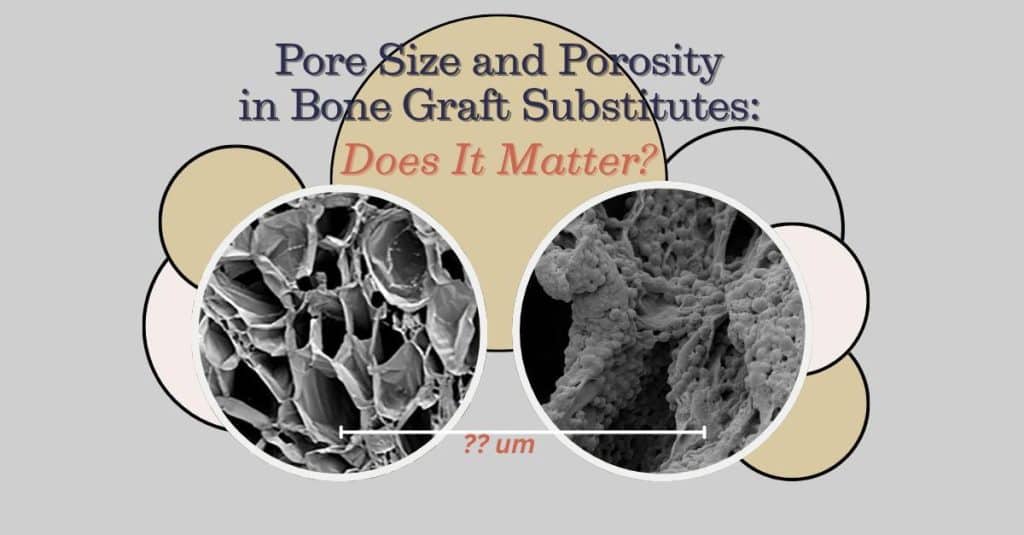
When engineering bone graft scaffolds, porosity and pore size are not interchangeable – and both matter.
The literature suggests that pores smaller than ~100 µm tend to fill with fibrous tissue rather than bone. A minimum pore size of ~100 µm is considered necessary for bone ingrowth, while pores in the 200–400 µm range appear optimal for osteogenesis, vascularization, and mineralization (Hing, 2005; Karageorgiou & Kaplan, 2005; Murphy O’Brien, 2010; ; Petrochenko & Narayan, 2010; Jiao et al., 2023). Pore sizes as large as 500–1,500 µm have been used experimentally, particularly where vascularization is paramount. However, increasing pore size can reduce initial mechanical strength and cell attachment, so careful design is required.
In short:
At Molecular Matrix, Inc., our novel Hyper-Crosslinked Carbohydrate Polymer (HCCP, commercial name Osteo-P® BGS) is engineered with pore sizes between 100-500 µm and a porosity of 75 – 95%. Osteo-P® BGS supports osteogenic cell infiltration and bone formation, even in the absence of added growth factors. For more information on how scaffold architecture affects bone healing, see www.molecularmatrix.com
Koleva, P. M., Keefer, J. H., Ayala, A. M., Lorenzo, I., Han, C. E., Pham, K., Ralston, S. E., Kim, K. D., & Lee, C. C. (2019). Hyper-Crosslinked Carbohydrate Polymer for Repair of Critical- Sized Bone Defects. BioResearch Open Access, 8(1), 111–120.
Hing, K. A. (2005). Bioceramic Bone Graft Substitutes: Influence of Porosity and Chemistry. International Journal of Applied Ceramic Technology, 2(3), 184–199. https://doi.org/10.1111/j.1744-7402.2005.02020.x
Jahir-Hussain, M. J., Maaruf, N. A., Esa, N. E. F., & Jusoh, N. (2021). The effect of pore geometry on the mechanical properties of 3D-printed bone scaffold due to compressive loading. IOP Conference Series: Materials Science and Engineering, 1051(1), 012016. https://doi.org/10.1111/j.1744-7402.2005.02020.x
Jiao, J., Hong, Q., Zhang, D., Wang, M., Tang, H., Yang, J., Qu, X., & Yue, B. (2023). Influence of porosity on osteogenesis, bone growth and osteointegration in trabecular tantalum scaffolds fabricated by additive manufacturing. Frontiers in Bioengineering and Biotechnology, 11, 1117954. https://doi.org/10.3389/fbioe.2023.1117954
Karageorgiou, V., & Kaplan, D. (2005). Porosity of 3D biomaterial scaffolds and osteogenesis. Biomaterials, 26(27), 5474–5491. https://doi.org/10.1016/j.biomaterials.2005.02.002
Murphy, C. M., & O’Brien, F. J. (2010). Understanding the effect of mean pore size on cell activity in collagen-glycosaminoglycan scaffolds. Cell Adhesion & Migration, 4(3), 377–381. https://doi.org/10.4161/cam.4.3.11747
Petrochenko, P., & Narayan, R. J. (2010). Novel Approaches to Bone Grafting: Porosity, Bone Morphogenetic Proteins, Stem Cells, and the Periosteum. Journal of Long-Term Effects of Medical Implants, 20(4), 303–315. https://doi.org/10.1615/JLongTermEffMedImplants.v20.i4.50
Yuan, H., Kurashina, K., De Bruijn, J. D., Li, Y., De Groot, K., & Zhang, X. (1999). A preliminary study on osteoinduction of two kinds of calcium phosphate ceramics. Biomaterials, 20(19), 1799–1806. https://doi.org/10.1016/S0142-9612(99)00075-7
© 2025 Molecular Matrix, Inc. All rights reserved.